Disorders of tibialis posterior tendon include:
• tenosynovitis
• tendinopathy
• partial and
• complete tears and
• rarely subluxation.
These abnormalities are most commonly encountered in the middle age female population. Clinically the patient complains of pain, clinical examination reveals tenderness over the tendon along with, as the disease progresses, flattening of the medial arch of the foot. Tibialis posterior tendon is a significant contributor to preservation of the medial arch and functions along with the spring ligament to preserve its integrity.
Tenosynovitis represents an early stage in tibialis posterior tendon disease. Look for
• fluid and synovial thickening
• increased blood flow
• Calibre changes
• Loss of internal structure
• Partial of full thickness defects
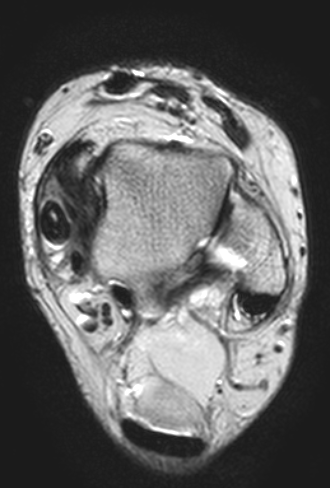
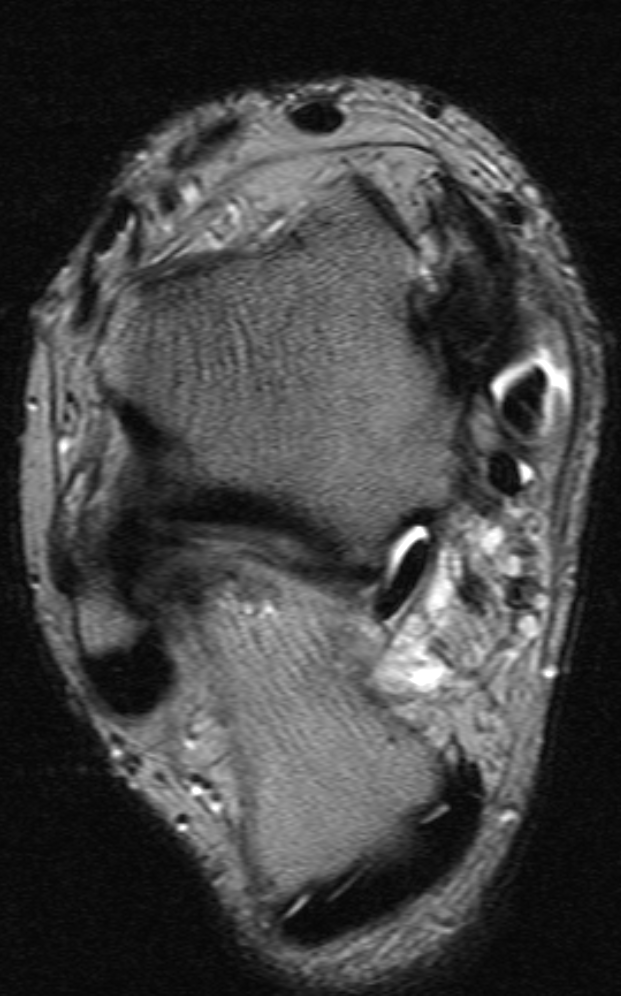
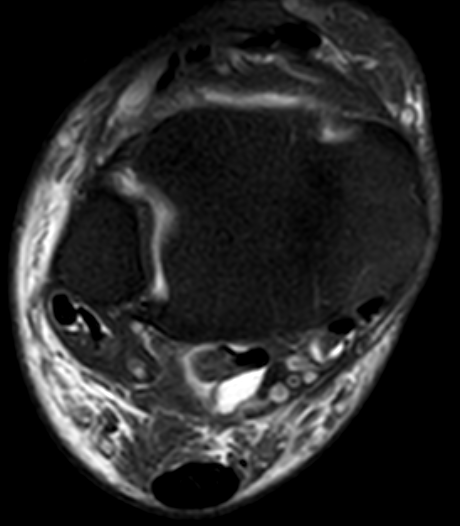
Note that a small quantity of fluid may be detected in the tendon sheath under normal circumstances. Depending on the position of the leg, fluid tends to gravitate in the sub-malleolar region. Normal fluid should not be conspicuous, nor should it show any complexity either on MR or ultrasound. Doppler ultrasound is also helpful in demonstrating increased blood flow. Various grades of tenosynovitis may be encountered. In some cases a significant synovial mass may form and indent or displace the tendon.Occasionally calcification can be identified within the tendon sheath. This is easier to detect on ultrasound and plain radiography than it is on MR. Patients with calcific tendinopathy often present with acute symptoms as crystal shedding can be particularly painful. Tibialis posterior tendon rupture can be partial or complete. Partial rupture takes two forms, one where the tendon is enlarged and another where it is atrophic. Hypertrophic tendinopathy is the commonest manifestation. As the name implies, the tendon is enlarged with areas of mucoid degeneration which manifesses intermediate signal on T1 weighted images and increased signal on T2. On ultrasound the tendon also appears enlarged with areas of decreased reflectivity associated with vascular ingrowth.